
Addison’s Disease: Understanding, Managing, and Living with Adrenal Insufficiency 2025 Guide
Addison’s disease, also known as primary adrenal insufficiency, is a rare but serious disorder that occurs when the adrenal glands fail to produce sufficient amounts of crucial hormones, particularly cortisol and, often, aldosterone. The adrenal glands, located on top of each kidney, are vital for hormone production that regulates metabolism, blood pressure, and the body’s response to stress.
Although Addison’s disease affects both men and women equally and can occur at any age, it is most commonly diagnosed in adults between the ages of 30 and 50.
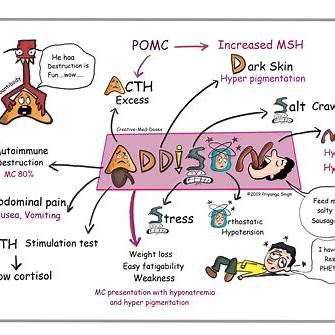
What Causes Addison’s Disease?
Several underlying factors can lead to adrenal insufficiency. The most common causes include:
Autoimmune Disorders
In developed countries, the majority of Addison’s cases result from autoimmune reactions where the immune system mistakenly attacks the adrenal cortex, the outer layer of the adrenal glands.
Infections
Tuberculosis (TB) remains a significant cause globally, while other infections such as fungal infections, HIV, and cytomegalovirus can also impair adrenal function.
Other Causes
- Adrenal gland tumors
- Genetic defects affecting adrenal development
- Hemorrhage or blood loss in the adrenal glands
- Long-term steroid therapy followed by abrupt withdrawal
Understanding the root cause is critical for developing a tailored treatment plan and long-term management.
Symptoms of Addison’s Disease
Addison’s disease symptoms can be subtle at first but often worsen over time if left untreated.
Early Symptoms
- Fatigue and muscle weakness
- Unexplained weight loss
- Loss of appetite
- Low blood pressure, particularly upon standing (orthostatic hypotension)
- Salt cravings
- Hyperpigmentation (darkening of the skin), especially in scars and skin folds
Advanced Symptoms
- Nausea, vomiting, and diarrhea
- Abdominal pain
- Depression and irritability
- Low blood sugar (hypoglycemia)
- Dehydration
Addisonian Crisis (Acute Adrenal Failure)
An Addisonian crisis is a medical emergency that requires immediate attention. Symptoms include:
- Severe pain in the lower back, abdomen, or legs
- Severe vomiting and diarrhea
- Dehydration leading to low blood pressure
- Loss of consciousness
Without prompt treatment, an Addisonian crisis can be fatal.
Diagnosis of Addison’s Disease
Diagnosing Addison’s disease involves a combination of clinical evaluation and laboratory testing.
Common Diagnostic Tests
- ACTH stimulation test: Measures how well the adrenal glands respond to adrenocorticotropic hormone.
- Blood tests: Check levels of sodium, potassium, cortisol, and ACTH.
- Imaging tests: CT scans of the adrenal glands can detect abnormalities like tumors or calcification.
Early and accurate diagnosis is vital for preventing complications and starting appropriate treatment.
Treatment Options for Addison’s Disease
Although Addison’s disease cannot be cured, it can be effectively managed with proper treatment.
Hormone Replacement Therapy
The cornerstone of Addison’s treatment is hormone replacement therapy to correct the levels of deficient hormones.
- Cortisol Replacement: Hydrocortisone, prednisone, or dexamethasone are commonly prescribed.
- Aldosterone Replacement: Fludrocortisone acetate is used to maintain sodium and potassium balance and manage blood pressure.
Lifestyle Modifications
- Stress Management: Patients must learn to adjust medication doses during periods of physical or emotional stress.
- Dietary Changes: A diet rich in sodium may be necessary for some patients, along with proper hydration.
- Medical Identification: Wearing a medical alert bracelet and carrying an emergency injection kit (e.g., Solu-Cortef) is recommended.
Monitoring and Regular Follow-ups
Patients need regular check-ups to adjust medication dosages and monitor for complications such as osteoporosis or infections.
Can Addison’s Disease Go Into Remission or Be Cured?
Is Remission Possible?
Unfortunately, Addison’s disease is not reversible. Once the adrenal cortex is damaged, it cannot regenerate. The disease is considered chronic and lifelong.
However, with consistent treatment and lifestyle adjustments, individuals with Addison’s can lead full, active lives.
Research and Advances
Current research is exploring regenerative medicine and gene therapy as potential future treatments, but as of 2025, no cure exists.
Managing stress, infections, and ensuring proper medication adherence can prevent complications and improve quality of life, but remission, in the classic sense, is not achievable.
Risks and Complications
Without proper management, Addison’s disease can lead to significant health risks.
Addisonian Crisis
As previously mentioned, a crisis is life-threatening and demands immediate medical care.
Long-Term Complications
- Cardiovascular issues due to low blood pressure
- Electrolyte imbalances
- Hypoglycemia
- Bone density loss from long-term corticosteroid use
- Chronic fatigue and reduced quality of life
Effective disease management is key to minimizing these risks.
Living with Addison’s Disease
Living with Addison’s disease requires vigilance, but many patients find a “new normal” with the right support and education.
Tips for Daily Management
- Stick to your medication schedule: Missing doses can be dangerous.
- Adjust for stress: Double or triple doses as prescribed during illnesses, surgeries, or injuries.
- Plan for emergencies: Keep an emergency injection kit handy.
- Stay educated: Regularly update yourself on new research and recommendations.
Support Systems
Joining support groups, either in-person or online, can provide emotional support and practical advice.
The Future for Patients with Addison’s Disease
Advancements in medical science are offering hope for easier and more effective management of Addison’s disease.
- Improved hormone formulations: Research is leading to longer-acting and more physiologically accurate hormone replacements.
- Wearable technologies: Devices to monitor cortisol levels in real-time are in development.
- Potential genetic therapies: Though still experimental, gene therapy could, one day, provide a cure.
Until then, patients must remain committed to their treatment regimen and stay informed about new developments.
Final Thoughts: Thriving with Addison’s Disease
While Addison’s disease is a serious, lifelong condition, modern treatments allow most patients to lead full and active lives. Awareness, proper medical management, and lifestyle adjustments make all the difference.
At present, Addison’s disease cannot go into remission or be healed completely, but its complications are highly manageable. With the right care team, proactive planning, and resilience, patients can thrive.
If you or a loved one is living with Addison’s disease, always prioritize education, preparedness, and support. The future is bright with ongoing research and innovation in adrenal health.

Early Signs of Addison’s Disease in Teens: What Parents Should Know – DateNightNow.com
[…] Addison’s Disease: Understanding, Managing, and Living with Adrenal Insufficiency 2025 Guide […]